Can you imagine this? It’s a normal day, and suddenly, you are pierced with a stabbing pain in your upper abdominal region like lightning. The pain is so intense that you double over, gasping and asking yourself if you need to go to the emergency room. This is how a gallbladder attack introduces itself – out of nowhere, severe, and completely terrifying for those who experienced it for the first time.
A gallbladder attack happens suddenly with intense abdominal pain and affects millions every year. New research suggests there is a very strong bidirectional relationship with fatty liver disease, where a gallbladder attack and fatty liver disease each increase the risk of having and developing the other via overlapping metabolic pathways. What most individuals don’t realise is that this painful, awful experience is often a sign of something deeper running in your body. This linkage may change the way you approach your overall health forever.
What is a Gallbladder Attack?
Your gallbladder might not seem like a significant organ hiding out underneath your liver, but it will sure get your attention if it misbehaves. A gallbladder attack, also known as acute cholecystitis, occurs when gallstones block the bile ducts, or if there is inflammation in this small but mighty organ. Consider your gallbladder as a holding area for bile which is the digestive juice produced by your liver to break down fats. When everything is working properly, the whole system behaves like a finely-tuned engine. When cholesterol gallstones form because your bile consists of too much cholesterol and too little bile salt to break it down, you could be in trouble.
During an attack, your gallbladder contracts against the blockage, producing waves of pain that can last for several hours.
It is your body’s painful and desperate effort to push through the obstruction, and you experience every second of that fight.
The 5 Signs of a Gallbladder Attack
1- Intense Upper Right Abdominal Pain
The defining aspect of any gallbladder attack is that recognizable pain in your upper right abdomen. Patients typically label the pain as sharp, cramping, or stabbing, though each of these labels significantly underestimates how the patient really feels. This is not a simple stomach ache that comes and goes.
The pain usually begins suddenly, it may spread to your right shoulder blade or, alternatively be located between your shoulder blades. It is constant and can last for minutes or several hours, and usually gets worse after eating fat. Most people find themselves holding their right side in an unconscious effort to try to relieve the pain.
2- Nausea and Vomiting
When your gallbladder cannot appropriately release bile, your entire digestive system is affected. Most gallbladder attacks are accompanied by continuous nausea, next often resulting in vomiting, which rarely provides relief. This happens because the body can’t reprocess the food being digested without enough bile flow. Nausea is more than just unpleasant; it’s a sign from your digestive system that something is very wrong. Patients often describe feeling nauseous even if they have not eaten. That is because disrupted bile flow affects the entire gastrointestinal system.
3- Fever and Chills
When someone has a gallbladder infection or severe inflammation, your body is sending out its internal alarm system. A fever over 101°F (38.3°C) with chills indicates your immune system is combating an infection, and that turns a painful problem into a medical emergency.
These systemic symptoms suggest acute cholecystitis and the need for immediate medical attention. Your body is telling you that what started as a blocked duct is now an infected organ requiring professional attention – and urgently.
4- Clay-Colored Stools and Dark Urine
Now, here is a place where it becomes visually alarming. If a person’s bile ducts are blocked, the bile cannot reach their intestines, where it gives stool its brown coloration. So the person will now have very light-colored or clay-colored stool that looks unlike normal.
At the same time, the person’s urine will become dark amber because bilirubin – a component of bile – is building up in the blood of the person, and getting filtered through the kidneys. Again, these changes in color are visible signs from the body showing that bile is not going where it should be.
5- Yellowing of Skin and Eyes (Jaundice)
Jaundice – when your skin and the whites of your eyes develop a yellowish hue – may be the most distressing finding to identify. It occurs when the bile duct is blocked, allowing bilirubin to accumulate in the bloodstream instead of being eliminated effectively. Jaundice usually first presents itself in the sclera (the whites of the eye), and then manifests itself in the skin. As soon as you recognize any yellowing, it is time to consult a doctor, as it suggests serious and urgent problems with your gallbladder.
The Connection Between Your Gallbladder and Liver
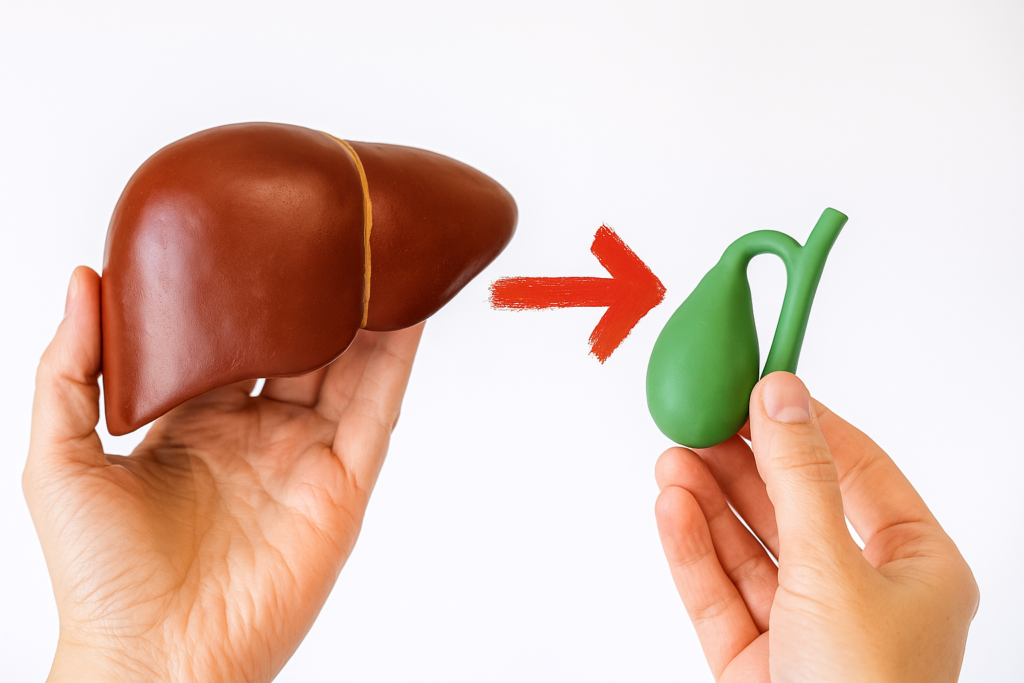
A gallbladder attack may not be isolated. Recent evidence has found a fascinating, and potentially troubling, connection between gallbladder and fatty liver diseases that we are just now beginning to understand.
These conditions may share common underlying drivers, such as obesity, insulin resistance, type 2 diabetes, and/or elevated cholesterol levels. These drivers create the conditions whereby both diseases could be developed concomitantly. In fact, studies have shown that an alarming 64.3% of women and 35.7% of men with gallstone disease also had fatty liver disease.
The Bidirectional Relationship
Research shows an impressive bidirectional relationship in which fatty liver disease increases the risk of gallstone disease formation by a factor of 1.26 times, while gallstones increase the risk of fatty liver disease by a factor of 1.14 times. It is almost like a metabolic dance, in which each disease increases the other’s risk.
In patients with fatty liver, the prevalence of gallstones is an average of 15-17%, which is significantly higher than in the general population, where only 5% of the population has them. This means if you have gallstones, you are at a higher risk of developing fatty liver disease.
How Cholesterol Metabolism Connects It All
We are only beginning to find the connection above, and there are also physiological connections well beyond shared risk factors. Fatty liver disease also alters normal cholesterol metabolism, being dumped into bile, supersaturating bile with cholesterol, and increasing gallstone formation. When liver cells have excess fat, they block excretion of bile, changing bile acid synthesis to produce bile that is more conducive towards precipitating cholesterol and forming cholesterol crystals.
So, this really could go on and on: the points about fatty liver can change how your body metabolizes cholesterol, which changes your bile, which drives the gallstone formation, which occurs in the gallbladder and ultimately elicits gallbladder attacks.
Gallbladder Treatment and Management

Emergency Management for Acute Attack
You will be focused on immediate relief from a gallbladder attack. Initial interventions will consist primarily of medications for pain and anti-nausea drugs. In most instances, the patient’s status will require hospitalization with intravenous fluids, fasting to rest the gallbladder, and antibiotics as needed if there is an infection.
Surgery
Laparoscopic cholecystectomy within one week of diagnosis of acute cholecystitis has now become standard of care in treatment. This procedure is considered minimally invasive and can be performed through small incisions to remove the gallbladder, halting future gallbladder attacks and allowing your liver to continue its normal function of producing bile.
Lifestyle Changes
Both gallbladder disease and fatty liver will respond to the same recommended lifestyle changes. Weight loss, low-fat diet, exercise, and management of diabetes will all promote similar change to the metabolic risk factors shared between both diseases. These recommendations are not merely a suggestion – but a necessary step to prevent future complications.
Following Up After Gallbladder Removal
If you’ve ever thought that removing your gallbladder cured your problems, then reconsider. Gallbladder removal (cholecystectomy) dramatically increases the risk of fatty liver disease by an estimated 1.97 times, especially in women. With a gallbladder removed, bile flows continuously into your intestines, disrupting normal enterohepatic circulation.
This disruption can influence the accumulation of triglycerides in your liver. Gallbladder removal (cholecystectomy) lowers levels of fibroblast growth factor 19 (FGF19), a hormone that normally helps regulate hepatic fatty acid synthesis. Without FGF19, your liver is generating and storing more triglycerides, contributing to a progressive state of fatty liver disease.
Prevention: Your Best Defence Strategy
Dietary Modifications that Make a Difference
A diet high in fiber, but low in saturated fats and cholesterol, may lower the risk of developing both gallstones and fatty liver. A Mediterranean diet pattern is especially helpful for overall metabolic health and liver function; think fresh vegetables, whole grains, lean proteins, and healthy fats like olive oil and nuts.
Regular Monitoring Can Save Your Life
If you have fatty liver disease, you should have gallbladder screening on a regular basis, while individuals with gallstones should consider liver function studies as well. Early identification allows for preventive measures to be taken before complications arise.
Gallbladder Symptoms You Can’t Ignore
If you experience severe abdominal pain for more than a few hours, or fever with chills, persistent vomiting, or jaundice, you should seek immediate medical evaluation. These complaints may suggest a serious complication that may require immediate medical attention, and your life may hinge on recognising these concerning symptoms.
With appropriate treatment, the majority of patients do get back to normal after a gallbladder attack. However, the connection between gallbladder attacks and fatty liver disease also allows for comprehensive treatment of both conditions, optimising metabolic health and quality of life.
Frequently Asked Questions

Does removal of the gallbladder increase the risk of a fatty liver?
Yes, cholecystectomy, ” Gallbladder removal”, increases the risk for fatty liver disease by 1.97 times, which is due to alterations in bile acids and a reduction of the hormone FGF19 that regulates liver fat metabolism.
How long does a gallbladder attack typically last?
A gallbladder attack can range from 30 minutes to several hours. The pain is often severe, and if symptoms persist beyond a few hours, you may need to seek emergency medical care.
Can you prevent both gallstones and fatty liver disease with diet?
Yes, by adhering to a low-fat, high-fiber diet and getting some exercise, you could diminish risk factors for both conditions by improving cholesterol metabolism and decreasing insulin resistance.
Recommended Products for Your Health Journey
- Digestive Enzymes with Bile Salts – Support healthy bile production and fat digestion post gallbladder removal.
- Milk Thistle Extract (Silymarin) – Traditional supplement for liver support management of fatty liver.
- Omega-3 Fish Oil. – Help reduce inflammation and support healthy liver function.
- Probiotic for Digestive Health – Helps maintain gut health post cholecystectomy, while supporting bile acid metabolism.
- Blood Glucose Monitor – Very important diabetes management if you have both.
Take Action and Share Your Journey
Suppose you are experiencing severe abdominal pain and have risk factors for gallbladder disease and fatty liver. In that case, it is essential to consult your health care provider to have a thorough assessment and personalized treatment plan. Your health journey matters, and understanding the possible interactions may lead to the prevention of serious complications that could arise.
Our reminder is to share this important information with your friends and family on social media. There may be a friend or family member experiencing these symptoms without understanding the connection. By sharing this information, you may help identify these warning signs.
Join our community here for weekly science-backed health tips, free meal plans, and carefully curated product recommendations delivered straight to your inbox!
Disclaimer:
This blog post is for informational purposes only and is not intended as medical advice. Always consult with a qualified healthcare professional before making any changes to your diet, exercise routine, or healthcare plan. The information provided is based on personal research and experience and may not apply to everyone