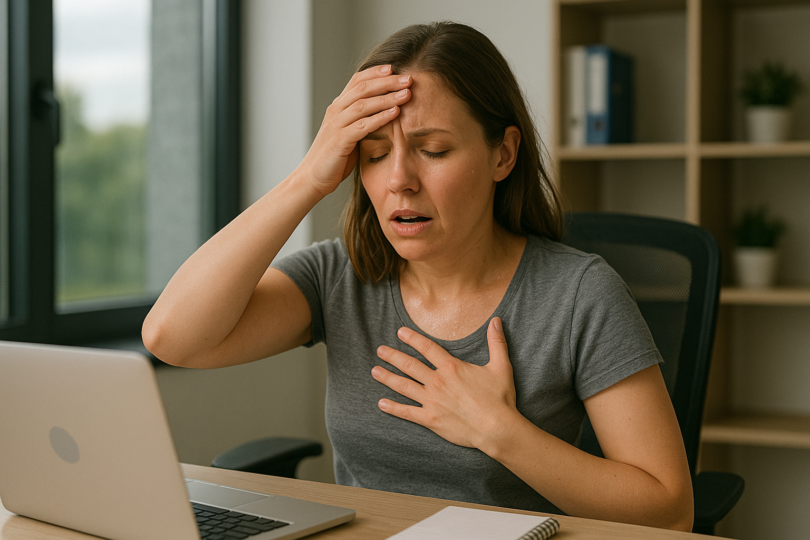
When your body gives you an SOS signal
You are at the office, and out of nowhere, the world seems as if it’s tilting. Your hands tremble as you grasp your coffee cup, your heart beats rapidly for no reason, and, as always, that familiar haze creeps into your head. If you are in your 40s, you would probably brush it off as stress, but your body is actually speaking to you in an important way about low blood sugar.
Low blood sugar, or hypoglycemia, is not a diabetic issue alone it reaches millions who are struggling with midlife’s complicated requirements. Whether experiencing career stress, family demands, or natural hormonal shifts, knowing how your blood sugar affects your life can be revolutionary. This post will show you how to identify signalling signs, grasp causes, and master your blood sugar levels with easy solutions tailored to your on-the-go schedule.
The Medical Definition of Low Blood Sugar
What Exactly Is Hypoglycemia?
Hypoglycemia is present if glucose levels are below 70 mg/dL (3.9 mmol/L). Normal glucose levels are between 80-130 mg/dL before meals and under 180 mg/dL two hours after a meal. Consider glucose top-shelf fuel for your body, particularly your brain, on which it uses 20% of your body’s energy. When they get low, it’s similar to running on empty. Your body activates alarm mechanisms, creating those uncomfortable feelings many people feel.
Dr. Sarah Chen, an endocrinologist at Cleveland Clinic, explains: “Your body has sophisticated mechanisms to maintain blood sugar balance. When glucose drops, your liver releases stored sugar, and your adrenal glands pump out hormones like adrenaline. These emergency responses cause many symptoms people feel during hypoglycemic episodes.” (Source: Diabetes Care, American Diabetes Association, 2024).
Types of Low Blood Sugar:
- Diabetic Hypoglycemia: From insulin or diabetes medications
- Non-Diabetic Hypoglycemia: Including reactive (after meals) and fasting types
Common Causes: Why Low Blood Sugar Happens
The Usual Suspects Responsible for Blood Sugar Drops
1- Missed or Delayed Meals
I would starve myself of necessary fuel by skipping my breakfasts and eating my lunch at work. By 3 p.m., I would be shaking and unable to focus.
2- Medication-Related Causes
- Too much insulin or diabetes medications
- Blood pressure medications affecting glucose metabolism
- Certain antibiotics and prescription drugs
- Over-the-counter medications combined with other factors
3- Exercise Without Proper Fuel
I would exercise without eating, assuming it would promote weight loss. As a result, I would get weak and dizzy for several hours.
4- Alcohol Consumption
Alcohol affects your liver’s release of glucose, particularly on an empty stomach. Impacts can take an extended period, i.e., even several hours.
5- Medical Conditions
- Liver disease affecting glucose storage
- Kidney disorders impacting medication clearance
- Hormonal imbalances (adrenal, thyroid issues)
- Gastric surgeries affecting food absorption
6- The Stress Connection

According to research at the Mayo Clinic, stress over a period has been known to cause irregular eating habits, unhealthy eating, disrupted sleep rhythms, as well as heightened inflammation. According to a Journal of Clinical Endocrinology & Metabolism study, stress-management methods lowered hypoglycemia episodes by 40% after 12 weeks.
All these factors contribute to fluctuations in blood sugar levels, more noticeably with age, as explained by the National Institute of Diabetes and Digestive and Kidney Diseases.
Identifying The Warning Signs From Your Body.
Early Symptoms: The First Wave
Physical Signs:
- Shakiness or trembling of hands
- Palpitations or rapid heartbeat
- Sweating, often including cold
- Immediate hunger sensations, Dizziness or lightheaded
- Weakness or sudden tiredness
Cognitive Signs:
- Focus problems
- Irritability or mood swings
- Feeling anxious or being on edge
- Frustration with easy tasks
- Feeling “spacey” or disconnected
Progressive Symptoms: When Things Get Serious
Moderate Symptoms:
- Blurred or double vision
- Slurred speech
- Clumsiness or poor coordination
- Severe headaches
- Nausea or vomiting
Severe Symptoms Requiring Immediate Attention:
- Severe confusion or disorientation
- Loss of consciousness
- Seizures
- Inability to eat or drink safely
Immediate Action: The 15-15 Rule and a Quick Solution
The Gold Standard: 15-15 Rule: If you notice symptoms, take prompt action:
- Eat 15 grams of rapid-acting carbohydrates
- Wait 15 minutes
- Test your blood sugar or check how you feel
- Repeat if symptoms continue
Most Effective
- 4 glucose tablets
- 1 tube glucose gel
- 15 g glucose powder in water
Common Alternatives:
- 1/2 cup juice from
- 1/2 cup regular soda
- 1 tablespoon honey or sugar
- 6-8 hard candies
Follow-Up Strategy
Once you recover, have a well-balanced snack with protein and complex carbohydrates to avoid another dip: apple with peanut butter, crackers and cheese, or Greek yogurt and berries
Prevention Strategies: Creating Long-Term Stability
Balanced Eating for Control

Meal Timing:
- Eat regular meals every 3-4 hours
- Never skip breakfast
- Have a balanced bedtime snack if required
- Plan snacks for longer intervals between meals
Balanced Meal Elements
- Lean protein (25%): chicken, fish, eggs, legumes
- Complex carbohydrates (25%): whole grains, sweet potatoes
- Non-starchy vegetables (50%): leafy greens, broccoli, peppers
- Healthy fats: avocado, olive oil, nuts in moderation
Read this blog post about healthy meals for overall meal planning that supports stable blood sugar.
Treatment with Medications
Key Points:
- Review all medications with your doctor regularly.
- Understand Timing Effects on Blood Sugar.
- Maintain medication logs for several prescriptions.
- Match Insulin Timing With Meals for Insulin Users
Monitoring Guidelines
- Anyone with diabetes or pre-diabetes
- People with frequent unexplained symptoms
- Those on blood sugar-affecting medications
- Individuals with family diabetes history
When to Seek Professional Help

Red Flag Symptoms
Contact healthcare providers for:
- Frequent episodes (more than 2-3 weekly)
- Severe episodes requiring assistance
- Unexplained episodes without diabetes
- Nighttime episodes that wake you
- Episodes not responding to treatment
Dr. Michael Rodriguez emphasizes: “Don’t wait until hypoglycemia becomes a pattern. Early intervention prevents complications and maintains better health.” Research from the New England Journal of Medicine shows early recognition and management reduces severe complication risk by 60%
Non-Diabetic Hypoglycemia: When It’s Not Diabetes
Reactive Hypoglycemia
It occurs 2-4 hours after eating, especially after high simple-carb meals. Your body overproduces insulin in response to blood sugar spikes.
Common Triggers:
- Large refined carbohydrate meals
- Sugary drinks on an empty stomach
- Processed high-sugar foods
- Irregular eating patterns
Hormonal Causes
Key Conditions:
- Adrenal insufficiency (impaired cortisol production)
- Growth hormone deficiency (affects glucose metabolism)
- Thyroid disorders (both hyper and hypothyroidism)
- Insulin-producing tumors (rare but serious)
Fasting Hypoglycemia
Blood sugar drops during food-free periods, caused by liver disease, kidney disease, certain medications, excessive alcohol, or critical illnesses.
Lifestyle Support: Daily Habits for Stability
Nutrition Strategies
Glycemic Index Focus:
- Low GI (55 or less): steel-cut oats, lentils, most vegetables
- Moderate GI (56-69): sweet potatoes, brown rice, whole grains
- Limit high GI (70+): white bread, sugary cereals, processed snacks
Anti-Inflammatory Eating: Chronic inflammation worsens blood sugar instability. Our comprehensive guide on Anti-Inflammatory Foods provides detailed strategies for incorporating these nutrients. Focus on:
- Fatty fish rich in omega-3s
- Colorful fruits and vegetables
- Nuts and seeds
- Herbs and spices (turmeric, ginger, cinnamon)
Research in the American Journal of Clinical Nutrition shows anti-inflammatory foods can improve insulin sensitivity and reduce blood sugar fluctuations by up to 25%.
Hydration and Supplements
Hydration Needs:
- 8-10 glasses water daily
- Extra fluids during exercise/heat
- Herbal teas as alternatives
- Limit blood sugar-swinging caffeine
Evidence-Based Supplements:
- Chromium (200-400 mcg): may improve glucose metabolism
- Alpha-lipoic acid: antioxidant supporting blood sugar control
- Cinnamon extract: may help glucose regulation
- Magnesium: essential for glucose metabolism
Always consult healthcare providers before starting supplements.
Stress Management and Exercise
Stress Reduction:
- Mindfulness meditation (10 minutes daily)
- Deep breathing during stressful moments
- Regular physical activity
- Maintain supportive relationships
Safe Exercise Practices:
- Check blood sugar before/during/after extended exercise
- Carry glucose tablets during workouts
- Exercise with a buddy when possible
- Plan post-workout snacks
“I learned to eat an apple with almond butter 30 minutes before gym sessions. It prevented shakiness and maintained consistent energy.”
Seizing the Future of Your Blood Sugar
Low blood sugar doesn’t need to dominate your existence during your 40s and after. By learning about causes, watching for signs, and taking effective prevention steps, you can have stable energy and overall well-being.
Key Takeaways:
- Recognition is power: Learn personal warning signs and act fast
- Prevention is better than treatment: Regular diet and habits prevent most attacks
- Professional assistance is important: Don’t be afraid to seek health professionals
- Individualized solutions are most effective: Tailor strategies for your particular circumstance
The process of achieving blood sugar stability is one that is never completed, but each step builds on the previous one. Whether you’re working with diabetes, reactive hypoglycemia, or unexplained crashes, you possess the tools and information needed to gain control.
Ready to begin? Start with one week of tracking symptoms and food habits these insights are invaluable into personal habits. Print off our complimentary Blood Sugar Tracking Sheet, or share your experience in the comments section. Your story could be all it takes for someone’s important first step towards improved health.
Have questions?
Talk with your healthcare provider about symptoms and create an individualized treatment plan. You’re not the only one millions of people control blood sugar problems on a daily basis, and you can too.
Is this helpful? Pass on this guide to friends and loved ones who could be of benefit. Let’s create a support community for blood sugar well-being together.
Join our community here for weekly science-backed health tips, free meal plans, and carefully curated product recommendations delivered straight to your inbox!
Disclaimer:
This blog post is for informational purposes only and is not intended as medical advice. Always consult with a qualified healthcare professional before making any changes to your diet, exercise routine, or healthcare plan. The information provided is based on personal research and experience and may not apply to everyone.